U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) Office of Regulatory Affairs (ORA)
July 2008 CGMP
美国卫生与公众服务部食品和药品管理局药物评价和研究中心(CDER)生物制品评价和研究中心(CBER)监管事务办公室(ORA)/2008年7月CGMP
This guidance is intended to assist in applying current good manufacturing practice (CGMP) required under section 501(a)(2)(B) of the Federal Food, Drug, and Cosmetic Act (FD&C Act) in the manufacture of most investigational new drugs (IND) used in phase 1 clinical trials. These drugs, which include biological drugs, are exempt from complying with 21 CFR part 211 under 21 CFR 210.2(c) (referred to as phase 1 investigational drugs).
Because a phase 1 clinical trial initially introduces an investigational new drug into human subjects, appropriate CGMP help ensure subject safety. This guidance applies, as part of CGMP, quality control (QC) principles to the manufacture of phase 1 investigational drugs (i.e., interpreting and implementing CGMP consistent with good scientific methodology), which foster CGMP activities that are more appropriate for phase 1 clinical trials, improve the quality of phase 1 investigational drugs, and facilitate the initiation of investigational clinical trials in humans while continuing to protect trial subjects.
This guidance replaces the guidance issued in 1991 titled Preparation of Investigational New Drug Products (Human and Animal) (referred to as the 1991 guidance) (Ref. 1) for the manufacture of phase 1 investigational drugs described in this guidance (see section III). However, the 1991 guidance still applies to the manufacture of investigational new products (human and animal) used in phase 2 and phase 3 clinical trials.
I. 简介
本指南旨在协助应用《联邦食品、药品和化妆品法》(FD&C法)第501(a)(2)(B)条所要求的现行良好生产规范(CGMP)来生产用于1期临床试验的大多数研究性新药(IND) 。这些药物,包括生物药物,根据21 CFR 210.2(c)条可免于遵守21 CFR第211部分(被称为第1期研究性药物)。
由于1期临床试验最初将研究性新药引入人体受试者,适当的CGMP有助于确保受试者安全。本指南作为CGMP的一部分,将质量控制(QC)原则应用于1期研究性药物的生产(即按照良好的科学方法解释和实施CGMP),促进更适合1期临床试验的CGMP活动,提高1期研究性药物的质量,并在继续保护受试者的同时促进人类研究性临床试验的启动。
本指南取代了1991年发布的题为《研究性新药产品(人类和动物)的制备》的指南(简称1991年指南),用于本指南所述的1期研究性药物的生产(见第三节)。然而,1991年的指导意见仍然适用于用于2期和3期临床试验的研究性新药产品(人类和动物)的生产。
This guidance applies to investigational new drug and biological products (including finished dosage forms used as placebos) intended for human use during phase 1 development that are subject to CGMP requirements of section 501(a)(2)(B) of the FD&C Act, and are excluded from complying with the CGMP regulations in 21 CFR part 211, by operation of 21 CFR 210.2(c). These include but are not limited to:
Investigational recombinant and non-recombinant therapeutic products
Vaccine products
Allergenic products
In vivo diagnostics
Plasma derivative products
Blood and blood components6
Gene therapy products
Somatic cellular therapy products (including xenotransplantation products).
本指南适用于在1期开发过程中拟供人类使用的研究性新药和生物制品(包括用作安慰剂的成品剂型),这些产品应符合《联邦药品管理法》第501(a)(2)(B)节的CGMP要求,并通过21 CFR 210.2(c)的操作,被排除在遵守21 CFR 211部分的CGMP法规之外。这些包括但不限于 :
研究性重组和非重组的治疗性产品
疫苗产品
过敏性产品
体内诊断法
血浆衍生物产品
血液和血液成分
基因治疗产品
体细胞治疗产品(包括异种移植产品)。
This guidance applies to phase 1 investigational drugs whether they are manufactured in small- or large-scale environments because phase 1 clinical trials (21 CFR 312.21(a)) are typically designed to assess tolerability, or feasibility, for further development of a specific drug or biological product. Furthermore, if an investigational drug has already been manufactured by an IND sponsor for use during phase 2 or phase 3 clinical trials or has been lawfully marketed, manufacture of such a drug must comply (21 CFR 211.1) with 21 CFR part 211 for the drug to be used in any subsequent phase 1 clinical trials, irrespective of the trial size or duration of dosing. See 21 CFR 210.2(c).
This guidance does not apply to the following phase 1 investigational products:
-
Human cell or tissue products regulated solely under § 361 of the Public Health Service Act
-
Clinical trials for products subject to the device approval or clearance provisions of the FD&C Act
-
Investigational products manufactured for phase 2 and phase 3 clinical trials
-
Already approved products that are being used during phase 1 clinical trials (e.g., for a new indication)
-
Positron Emission Topography (PET) drugs that are subject to § 501(a)(2)(C) of the FD&C Act and/or the new PET CGMP in 21 CFR part 212 when finalized
If you need clarification on the applicability of this guidance to a specific clinical trial, contact the appropriate FDA Center with responsibility for review of the IND.
本指南适用于1期研究性药物,无论它们是在小型或大型环境中生产,因为1期临床试验(21 CFR 312.21(a))通常是为了评估特定药物或生物制品的进一步发展的耐受性或可行性。此外,如果一种研究性药物已经由IND申请人成产,用于2期或3期阶段的临床试验,或者已经合法上市,那么这种药物的制造必须符合(21 CFR 211.1)21 CFR第211部分的规定,才能用于随后的任何第1阶段临床试验,而不考虑试验规模或用药时间。见21 CFR 210.2(c)。
-
仅受《公共卫生服务法》第361条监管的人类细胞或组织产品
-
受《FD&C法案》设备批准或许可条款约束的产品的临床试验
-
为2期和3期临床试验制造的研究性产品
注释:此类药物的生产必须符合21 CFR第211部分中用于后续任何一期临床试验的药物的适当章节,无论试验规模或给药时间。
-
在1期临床试验中使用的已经批准的产品(例如,用于新的适应症)。
-
受《FD&C法案》第501(a)(2)(C)条和/或最终确定的21 CFR第212部分中新的PET CGMP约束的正电子发射拓扑(PET)药物。
如果您需要澄清本指南对特定临床试验的适用性,请联系负责审查IND的相应FDA中心。
This guidance is applicable to all manufacturers of phase 1 investigational drugs, including contractors and other specialized service providers as well as IND sponsors who participate in any aspect of manufacturing.
We (FDA) recommend that you use this guidance as a companion to other FDA guidance documents describing the chemistry, manufacturing, and control (CMC) information submitted and reviewed in an IND application for phase 1 clinical trials . In many cases, at this stage of development manufacture of the active pharmaceutical ingredient and the phase 1 investigational drug will be accomplished through a series of steps within a single facility. Manufacturers of new active pharmaceutical ingredients (also referred to as API or drug substance) must also conform with CGMP as required in § 501(a)(2)(B) of the FD&C Act. Limited guidance is available on CGMP for the manufacture of new API in some IND products (Ref. 3). Manufacturers of APIs should implement CGMP appropriate to the stage of clinical development and consider the recommendations described in this guidance for the manufacture of APIs used in phase 1 investigational drugs.
本指南适用于所有临床1期阶段研究性药物的制造商,包括承包商和其他专业服务提供商以及参与生产的任何方面的IND申请人。
我们(FDA)建议您将本指南作为其他FDA指南文件的补充,描述在1期临床试验的IND申请中提交和审查的化学、制造和控制(CMC)信息。在许多情况下,在这个开发阶段,活性药物成分和1期临床试验阶段研究药物的制造将在一个设施内通过一系列的步骤完成。新的活性药物成分(也被称为API或药物物质)的制造商也必须符合《FD&C法案》第501(a)(2)(B)条的要求,遵守CGMP。在一些IND产品中,对新的API的生产提供了有限的CGMP指导。API的制造商应实施与临床开发阶段相适应的CGMP,并考虑本指南中描述的用于1期研究性药物的API制造的建议。
IV. GENERAL GUIDANCE FOR COMPLYING WITH THE STATUTE
This guidance provides recommendations that manufacturers of phase 1 investigational drugs can use to comply with the statutory requirement for CGMP under § 501(a)(2)(B) of the FD&C Act. Manufacturers should also consult other resources, such as literature and technical bulletins for additional detailed information on CGMP that complement the approaches and recommendations in this guidance.
During product development, the quality and safety of phase 1 investigational drugs are maintained, in part, by having appropriate QC procedures in effect. Using established or standardized QC procedures and following appropriate CGMP will also facilitate the manufacture of equivalent or comparable IND product for future clinical trials as needed.
IV. 遵守法规的一般指导
本指南提供了1期研究用药的制造商可以用来遵守《联邦药品管理法》第501(a)(2)(B)条对CGMP的法定要求的建议。制造商还应该查阅其他资源,如文献和技术公报,以获得有关CGMP的更多详细信息,以补充本指南中的方法和建议。
在产品开发过程中,1期研究性药物的质量和安全部分是通过实施适当的质量控制程序来维持的。使用已建立的或标准化的质量控制程序并遵循适当的CGMP,也将有助于在需要时为未来的临床试验生产同等或可比的IND产品。
Adherence to CGMP during manufacture of phase 1 investigational drugs occurs mostly through:
-
Well-defined, written procedures
-
Adequately controlled equipment and manufacturing environment
-
Accurately and consistently recorded data from manufacturing (including testing)
Manufacturers may have acceptable alternatives to meet the objectives described in this guidance. It is the manufacturer’s responsibility to provide and use such methods, facilities, and manufacturing controls to ensure that the phase 1 investigational drug meets appropriate standards of safety, identity, strength, quality, and purity. Manufacturers of phase 1 investigational drugs should consider carefully how to best ensure the implementation of standards, practices, and procedures that conform to CGMP for their specific product and manufacturing operation.
在1期临床试验药物的生产过程中,对CGMP的遵守主要通过:
制造商可能有可接受的替代方法来满足本指南中描述的目标。制造商有责任提供和使用这种方法、设施和制造控制,以确保第1期研究性药物符合适当的安全、鉴别、剂量、质量和纯度标准。1期临床试验药物制造商应仔细考虑如何确保其特定产品和生产操作符合CGMP的标准、规范和程序的执行。
In applying appropriate CGMP, we recommend that manufacturers consider carefully the hazards and associated risks from the manufacturing environment that might adversely affect the quality of a phase 1 investigational drug, especially when the phase 1 investigational drug is manufactured in laboratory facilities that are not expressly or solely designed for their manufacture. For example, of particular importance is the susceptibility of a phase 1 investigational drug to contamination or cross contamination with other substances (e.g. chemicals, biologicals, adventitious agents) that may be present from previous or concurrent research or manufacturing activities.
We recommend the following steps to establish the appropriate manufacturing environment for phase 1 investigational drugs:
-
A comprehensive and systematic evaluation of the manufacturing setting (i.e., product environment, equipment, process, personnel, materials) to identify potential hazards
-
Appropriate actions prior to and during manufacturing to eliminate or mitigate potential hazards to safeguard the quality of the phase 1 investigational drug
在应用适当的CGMP时,我们建议生产商仔细考虑来自生产环境的危险和相关风险,这些危险和风险可能对1期研究性药物的质量产生不利影响,特别是当1期研究性药物是在并非明确或专门为其生产而设计的实验室设施中生产时。例如,特别重要的是,1期研究性药物是否容易受到以前或同时进行的研究或生产活动中可能存在的其他物质(如化学品、生物制品、不定因素)的污染或交叉污染。
我们建议采取以下步骤,为第1期研究性药物建立适当的生产环境:
-
对生产环境(即产品环境、设备、工艺、人员、材料)进行全面和系统的评估,以确定潜在的危险性
-
在生产前和生产过程中采取适当行动,消除或减轻潜在危害,以保障1期研究性药物的质量
Any manufacturing environment, including a laboratory, should have adequate work areas that are properly equipped and controlled for the specific operation(s) needed to manufacture a phase 1 investigational drug. Given the diversity of products and requisite manufacturing operations, not all environments may be acceptable for the manufacture of the specific phase 1 investigational drug under consideration. In these situations, you should use more suitable facilities.
A number of technologies and resources are available that can facilitate conformance with CGMP and streamline product development. Some examples include:
-
Use of disposable equipment and process aids to reduce cleaning burden and chances of contamination
-
Use of commercial, prepackaged materials (e.g., Water For Injection (WFI), pre-sterilized containers and closures) to eliminate the need for additional equipment or for demonstrating CGMP control of existing equipment
-
Use of closed process equipment (i.e., the phase 1 investigational drug is not exposed to the environment during processing) to alleviate the need for stricter room classification for air quality
-
Use of contract or shared CGMP manufacturing facilities and testing laboratories (including specialized services). For example, some academic institutions have developed shared manufacturing and testing facilities that can be used by institutional sponsors.
任何生产环境,包括实验室,都应该有足够的工作区域,适当的设备和控制,用于生产1期临床试验药物所需的特定操作。考虑到产品的多样性和必要的生产操作,并不是所有环境都可以用于正在考虑的特定1期研究药物的生产。在这种情况下,您应该使用更合适的设施。
有许多技术和资源可以促进对CGMP的遵守并简化产品开发。一些例子包括:
使用一次性设备和工艺辅助工具,以减少清洁负担和污染的机会
使用商业预包装材料(例如,注射用水(WFI)、预消毒容器和封口),以消除对额外设备的需求或证明对现有设备的CGMP控制
使用封闭式加工设备(即第一阶段研究性药物在加工过程中不暴露在环境中)以减轻对空气质量进行更严格的房间分类的需要
使用合同或共享的CGMP生产设施和测试实验室(包括专业服务)。例如,一些学术机构已经开发了共享的生产和测试设施,可供机构赞助商使用。
Under CGMP, if a sponsor or manufacturer initiates a contract with another party to perform part or all of the phase 1 investigational drug manufacturing, the sponsor or manufacturer, and contractor are both responsible for assuring that the phase 1 investigational drug is manufactured in compliance with CGMP. This assurance is achieved, in part, by having effective quality control functions (see section V.B). We recommend that the manufacturer or sponsor assess the contractor to ensure that effective quality control functions are in place.
根据CGMP,如果申请人或制造商与另一方签订合同,执行部分或全部1期研究性药物的生产,发起人或制造商和承包商都有责任保证1期研究性药物的生产符合CGMP的规定。这种保证部分是通过有效的质量控制功能实现的。我们建议制造商或赞助商对承包商进行评估,以确保有效的质量控制功能到位。

V. RECOMMENDED CGMP FOR PHASE 1 INVESTIGATIONAL DRUGS ( 建议的1期研究性药物的CGMP )
Consistent with the FD&C Act (§ 501(a) (2) (B)), CGMP must be in effect for the manufacture of each batch of investigational drug used during phase 1 clinical trials. Manufacturers should establish manufacturing controls based on identified hazards for the manufacturing setting that follow good scientific and QC principles. The following manufacturing controls are applicable to the manufacture of phase 1 investigational drugs and in some specific manufacturing situations. These recommendations provide flexibility to the manufacturers in implementing CGMP controls appropriate to their specific situation and application.
根据FD&C法案(第501(a)(2)(B)条),在1期临床试验中使用的每批研究性药物的生产必须实行CGMP。制造商应根据已确定的制造环境的危险性建立制造控制,遵循良好的科学和质量控制原则。以下制造控制措施适用于1期研究性药物的制造和一些特定的制造情况。这些建议为制造商实施适合其具体情况和应用的CGMP的控制提供了灵活性。
A. Personnel (人员)
All personnel should have the education, experience, and training or any combination thereof to enable each individual to perform their assigned function. In particular, personnel should have the appropriate experience to prepare the phase 1 investigational drug and be familiar with QC principles and acceptable methods for complying with the statutory requirement of CGMP, such as the recommendations described in this guidance.
所有人员应具有教育、经验和培训或其任何组合,以使每个人能够履行其指定的职能。特别是,人员应该有适当的经验来准备1期临床试验药物,并熟悉QC原则和可接受的方法来遵守CGMP的法定要求,如本指南中描述的建议。
B. QC Function (质控功能)
Every manufacturer should establish a written plan that describes the role of and responsibilities for QC functions.8 For example, a written plan should provide, at a minimum, for the following functions.
Responsibility for examining the various materials used in the manufacture of a phase 1 investigational drug (e.g., containers, closures, in-process materials, raw materials, packaging materials, and labeling) to ensure that they are appropriate and meet defined, relevant quality standards
Responsibility for review and approval of manufacturing procedures, testing procedures, and acceptance criteria
Responsibility for releasing or rejecting each batch of phase 1 investigational drug based on a cumulative review of completed manufacturing records and other relevant information (e.g., procedures were followed, product tests performed appropriately, acceptance criteria met)
Responsibility for investigating unexpected results or errors that occur during manufacturing or from complaints received and initiation of corrective action, if appropriate.
Although quality is the responsibility of all personnel involved in manufacturing, we recommend that you assign an individual(s) to perform QC functions independent of manufacturing responsibilities, especially for the cumulative review and release of phase 1 investigational drug batches.
每个制造商都应制定一个书面计划,描述QC职能的作用和责任。例如,一个书面计划至少应规定以下职能。
-
负责检查1期研究性药物生产中使用的各种材料(如容器、封闭物、加工中的材料、原材料、包装材料和标签),以确保它们是合适的,并符合规定的相关质量标准 。
-
-
负责根据对已完成的生产记录和其他相关信息(例如,程序得到遵守,产品测试适当进行,符合验收标准)的累积审查,释放或拒绝每一批第一阶段的研究性药物
-
负责调查制造过程中发生的或从收到的投诉中出现的意外结果或错误,并酌情启动纠正措施。
虽然质量是所有参与生产的人员的责任,但我们建议您指定一个人独立于生产职责执行QC职能,特别是1期临床试验药品批次的累计审核和放行。
However, in very limited circumstances and depending on the size and structure of an organization, all QC functions may be performed by the same individual(s) performing manufacturing. For example, in some small operations, it may be necessary to have the same individual perform both manufacturing and QC functions, including release or rejection of each batch. However, in such circumstances, we strongly recommend that another qualified individual not involved in the manufacturing operation conduct an additional periodic review of manufacturing records and other QC activities.
When activities such as testing, commonly performed by dedicated QC personnel in commercial manufacture, are performed by manufacturing personnel in phase 1 studies, adequate controls should be in place (e.g., segregation of testing from manufacturing) so as to not contaminate testing or negatively affect test results.
但是,在非常有限的情况下,根据一个组织的规模和结构,所有的QC职能可以由从事生产的同一个人完成。例如,在一些小型企业中,可能有必要让同一个人同时执行制造和QC职能,包括每批产品的放行或拒绝。但是,在这种情况下,我们强烈建议由另一个不参与生产操作的合格人员对生产记录和其他QC活动进行额外的定期审查。
当商业生产中通常由专门的QC人员进行的测试等活动在1期阶段研究中由生产人员进行时,应该有足够的控制措施(例如,测试与生产分离),以便不污染测试或对测试结果产生负面影响。
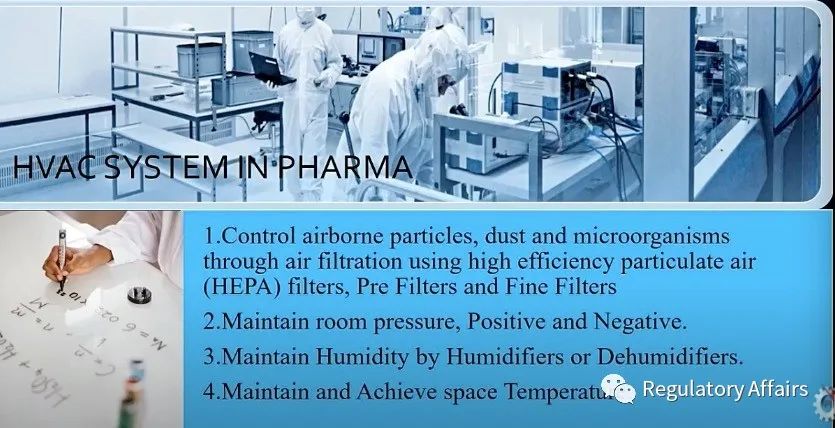
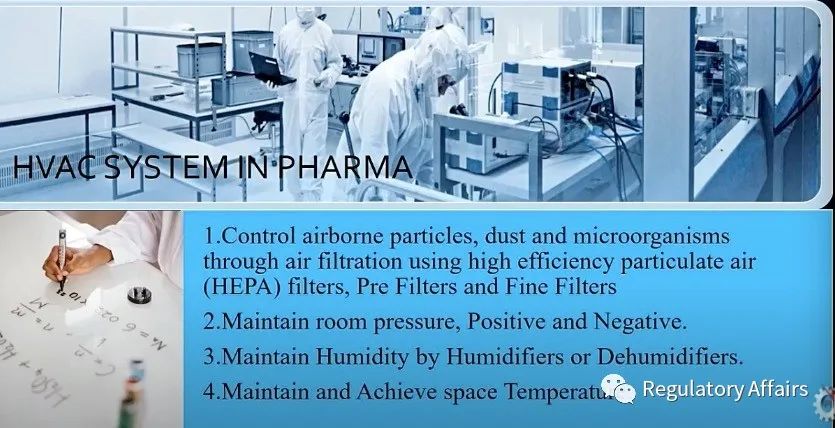
C. Facility and Equipment
Any facility used for manufacturing phase 1 investigational drugs should have adequate work areas and equipment for the intended task.
Each facility should provide the following described work area and equipment:
Sufficient space, clean environment, appropriate construction
Appropriate lighting, ventilation, and heating
Appropriate cooling, plumbing, washing, and sanitation
Appropriate equipment to maintain an air cleanliness classification suitable to the operation performed in the area. For example, appropriate air handling systems (e.g., laminar flow hoods) to aid in preventing contamination and cross-contamination of the phase 1 investigational drug.
Appropriate equipment that will not contaminate the phase 1 investigational drug or otherwise react with, add to, or be absorbed by the phase 1 investigational drug; and that is properly maintained, calibrated, cleaned, and sanitized at appropriate intervals following written procedures.
We recommend that you identify all equipment used for a particular process and document such use in the manufacturing record. You should follow the provisions described under Sterile Products/Aseptically Processed Products (see section VI.C) for phase 1 investigational drugs prepared using aseptic processing.
Use of procedural controls in a facility promotes orderly manufacturing and aids in preventing contamination, cross contamination and mix-ups (see section VI.A).
任何用于生产1期研究性药物的设施都应该有足够的工作区域和设备来完成预定的任务。
-
-
-
-
-
适当的设备,以保持适合在该区域进行的操作的空气清洁度分类。例如,适当的空气处理系统(如层流罩),以帮助防止第一阶段调查药物的污染和交叉污染。
-
适当的设备,不会污染第1期研究性药物或以其他方式与第1期研究性药物发生反应、添加或被其吸收;并按照书面程序以适当的时间间隔进行适当的维护、校准、清洁和消毒。
我们建议您确定用于特定工艺的所有设备,并在生产记录中记录这种用途。对于使用无菌加工制备的1期研究性药物,您应遵循无菌产品/无菌加工产品(见第VI.C节)中所述的规定。
在设施中使用程序控制可以促进有序的生产,并有助于防止污染、交叉污染和混合(见第VI.A节)
D. Control of Components, and Containers and Closures
You should establish written procedures describing the handling, review, acceptance, and control of material (i.e., components, containers, closures) used in the manufacture of a phase 1 investigational drug. Materials should be controlled (e.g., segregated, labeled) until you have examined or tested the materials, as appropriate, and released them for use in manufacturing. It is important to handle and store such materials in a manner that prevents degradation or contamination.
The manufacturer should be able to identify and trace all materials used in the manufacture of a phase 1 investigational drug from receipt to use in the manufacture of each batch. We recommend that you keep a record (e.g., log book) containing relevant information on all materials. At a minimum, recorded relevant information would include receipt date, quantity of the shipment, supplier's name, material lot number, storage conditions, and corresponding expiration date.
The manufacturer should establish acceptance criteria for specified attributes on each material. For some materials, all relevant attributes or acceptance criteria may not be known at the phase 1 stage of product development. However, attributes and acceptance criteria selected for assessment should be based on scientific knowledge and experience for use in the specific phase 1 investigational drug. The material attributes and acceptance criteria will be reviewed in the IND application (Refs. 1 through 6).
We recommend that you examine the certificate of analysis (COA) and/or other documentation on each lot of material to ensure that it meets established acceptance criteria for specified attributes. For some (e.g., human and animal derived material), documentation should include information on sourcing and/or test results for adventitious agents, as appropriate. If documentation for a material is incomplete for a specified attribute, we recommend that you test for the incomplete specified attribute of the material. For each batch of the API (or drug substance), you should perform confirmatory identity testing.
您应制定书面程序,说明用于生产1期研究性药物的材料(即成分、容器、封盖)的处理、审查、接受和控制。材料应受到控制(例如,隔离、贴标签),直到您酌情检查或测试材料,并将其用于生产。重要的是,处理和储存这些材料的方式应能防止降解或污染。
制造商应能识别和追踪用于生产1期研究性药物的所有材料,从接收到用于制造每一批产品。我们建议你保留一份记录(如日志),包含所有材料的相关信息。至少,记录的相关信息应包括收货日期、装运数量、供应商名称、材料批号、储存条件和相应的失效日期。
制造商应该为每种材料的特定属性制定验收标准。对于某些材料,在产品开发的1期可能还不知道所有相关属性或验收标准。然而,为评估而选择的属性和验收标准应以科学知识和经验为基础,用于特定的第1阶段研究性药物。材料属性和验收标准将在IND申请中审查(参考文献1至6)。
我们建议您检查每批材料的分析证书(COA)和/或其他文件,以确保其符合指定属性的既定验收标准。对于某些材料(如人类和动物来源的材料),文件应酌情包括来源信息和/或不定因素的测试结果。如果某种材料的文件在某一特定属性方面不完整,我们建议您对该材料的不完整特定属性进行测试。对于每一批原料药(或药物物质),您应该进行确认性测试。
The manufacture of phase 1 investigational drugs should follow written manufacturing and process control procedures that provide for the following records.
A record of manufacturing data that details the materials, equipment, procedures used, and any problems encountered during manufacturing. We recommend that manufacturers retain records sufficient to replicate the manufacturing process. Similarly, if the manufacture of a phase 1 investigational drug batch is initiated but not completed, we recommend that the record include an explanation of why manufacturing was terminated.
A record of changes in procedures and processes used for subsequent batches along with the rationale for any changes.
A record of the microbiological controls that have been implemented (including written procedures) for the production of sterile-processed phase 1 investigational drugs that are covered by this guidance. You should follow the recommendations for use of aseptic techniques and the control of in-process materials, components, and container closures designed to prevent microbial and endotoxin contamination (see section VI.C).
1期临床研究性药物的生产应遵循书面的生产和工艺控制程序,规定以下记录:
生产数据记录,详细说明所使用的材料、设备、程序,以及制造过程中遇到的任何问题。我们建议制造商保留足以复制生产过程的记录。同样,如果一期研究性药物批次的生产已经开始但没有完成,我们建议该记录包括对生产终止原因的解释。
后续批次使用的程序和工艺的变化记录,以及任何变化的理由。
为生产本指南所涉及的无菌加工的1期临床研究性药物而实施的微生物控制的记录(包括书面程序)。您应遵循关于使用无菌技术和控制加工中的材料、部件和容器封口的建议,以防止微生物和内毒素污染(见第六章C节)。
F. Laboratory Controls (实验室控制 )
Laboratory tests used in manufacturing (e.g., testing of materials, in-process material, packaging, drug product) should be scientifically sound (e.g., specific, sensitive, and accurate), suitable and reliable for the specified purpose. You should perform tests under controlled conditions and follow written procedures describing the testing methodology. You should maintain records of all test results, procedures, and changes in procedures.
在生产过程中使用的实验室测试(例如,材料、中控、包装、药品的测试)应该在科学上是合理的(例如,特定的、敏感的和准确的),对特定的目的是合适的和可靠的。您应在受控条件下进行测试,并遵循描述测试方法的书面程序。您应保持所有测试结果、程序和程序变化的记录。
You should perform laboratory testing of the phase 1 investigational drug to evaluate quality attributes including those that define the identity, strength, potency, purity, as appropriate. Specified attributes should be monitored, and acceptance criteria applied appropriately. For known safety-related concerns, specifications should be established and met. For some phase 1 investigational drug attributes, all relevant acceptance criteria may not be known at this stage of development. This information will be reviewed in the IND submission (Refs. 1 through 6).
您应该对1期临床研究性药物进行实验室测试,以评估质量属性,包括那些定义身份、强度、效力、纯度的质量属性,视情况而定。应监测指定的属性,并适当地应用验收标准。对于已知的与安全有关的问题,应制定并满足规范。对于一些1期研究性药物属性,在这个开发阶段可能还不知道所有相关的验收标准。这些信息将在提交的IND中审查(参考文献1至6)。
To ensure reliability of test results, we recommend that you calibrate laboratory equipment at appropriate intervals and maintain the equipment according to established written procedures. We recommend that personnel verify that the equipment is in good working condition when samples are analyzed (e.g., system suitability).
为了确保测试结果的可靠性,我们建议您以适当的时间间隔校准实验室设备,并按照既定的书面程序维护设备。我们建议人员在分析样品时核实设备是否处于良好的工作状态(例如,系统适用性)。
You should retain a representative sample from each batch of phase 1 investigational drug. We recommend retention of both the API and phase 1 investigational drug in containers used in the clinical trials. When feasible, we recommend that the sample consist of a quantity adequate to perform additional testing or investigation if required at a later date (e.g., twice the quantity necessary to conduct release testing, excluding testing for pyrogenicity and sterility). We recommend that you appropriately store and retain the samples for at least two years following clinical trial termination, or withdrawal of the IND application.
您应从每批1期研究性药物中保留一个有代表性的样品。我们建议在临床试验中使用的容器中同时保留原料药和1期研究性药物。在可行的情况下,我们建议样品的数量应足以在以后需要时进行额外的测试或调查(例如,进行释放测试所需数量的两倍,不包括热原性和无菌性测试)。我们建议您在临床试验终止或撤回IND申请后,适当地储存和保留样品至少两年时间。
We recommend initiation of a stability study using representative samples of the phase 1 investigational drug to monitor the stability and quality of the phase 1 investigational drug during the clinical trial (i.e., date of manufacture through date of last administration)
我们建议启动稳定性研究,使用具有代表性的1期研究性药物样本,监测1期研究性药物在临床试验期间的稳定性和质量(即从生产日期到最后给药日期)。
G. Packaging, Labeling and Distributing (包装、标签和分发 )
The phase 1 investigational drug should be suitably packaged to protect it from alteration, contamination, and damage during storage, handling, and shipping. You should establish written procedures for controlling packaging, labeling, and distribution operations. We recommend the use of appropriate measures (e.g., product segregation, label reconciliation, verify operations by a second person, confirmatory laboratory testing, QC review) to achieve effective control especially in situations where the potential for mix-ups is more likely (e.g., use of placebo, blinded trials, multiple strengths).
1期研究性药物应进行适当的包装,以保护其在储存、处理和运输过程中不被改变、污染和损坏。您应制定书面程序来控制包装、标签和分销业务。我们建议使用适当的措施(例如,产品隔离、标签核对、由第二个人核实操作、确认性实验室测试、质量控制审查)来实现有效控制,特别是在更有可能发生混淆的情况下(例如,使用安慰剂、盲法试验、多种强度)。
As it relates to phase 1 clinical trials, distribution includes the transport of a phase 1 investigational drug covered by this guidance to clinical investigators. You should handle phase 1 investigational drugs in accordance with labeled conditions (e.g., temperature) to ensure retention of the quality of the product. A distribution record of each batch of phase 1 investigational drug must be sufficiently detailed to allow traceability and facilitate recall of the phase 1 investigational drug if necessary (§ 312.57(a))
由于与一期临床试验有关,分发包括将本指南所涉及的一期研究性药物运送给临床研究人员。您应按照标注的条件(如温度)处理1期研究性药物,以确保保留产品的质量。每批1期研究用药的配送记录必须足够详细,以便于追踪,并在必要时便于召回第1期研究用药(§312.57(a))。
H. Recordkeeping (记录保存 )
As indicated in previous sections, manufacturers should keep complete records relating to the quality and operation of the manufacturing processes, including but not limited to:
-
Equipment maintenance and calibration
-
Manufacturing records and related analytical test records
-
-
QC functions (as defined in section V.B)
-
-
Deviations and investigations
-
Under § 312.57(c), sponsors must retain records for at least two years after a marketing application is approved for the drug, or if an application is not approved for the drug, until two years after shipment and delivery of the drug for investigational use is discontinued and FDA is notified.
如前几节所述,制造商应保存与生产过程的质量和操作有关的完整记录,包括但不限于:
根据312.57(c)条,申请人必须在药物的上市申请被批准后至少保留两年的记录,如果药物的申请没有被批准,则在用于研究用途的药物的运输和交付停止并通知FDA后两年内保留记录。
VI. SPECIAL MANUFACTURING SITUATIONS (特殊制造情况 )
A. Multi-Product Facilities (多产品设施 )
We recommend that you manufacture only one phase 1 investigational drug at any given time, in an area or room separate from unrelated activities. However, you could use the same area or room for multiple purposes, including manufacture of other investigational products or laboratory research, provided that appropriate cleaning and procedural controls are in place to ensure that there is no carry-over of materials or products, or mix-ups. In such cases, the design or layout of an area should promote the orderly handling of materials and equipment, the prevention of mix-ups, and the prevention of contamination of equipment or product by substances, previously manufactured products, personnel, or environmental conditions.
我们建议您在任何时候都只生产一种1期的研究性药物,并在一个与不相关的活动分开的区域或房间内。但是,你可以将同一区域或房间用于多种用途,包括生产其他研究性产品或实验室研究,但必须有适当的清洁和程序控制,以确保没有材料或产品的遗留,或发生混淆。在这种情况下,一个区域的设计或布局应促进材料和设备的有序处理,防止混淆,并防止物质、先前制造的产品、人员或环境条件对设备或产品的污染。
Examples of procedural controls could include procedures for clearing the room of previous product materials, product segregation, component segregation, and use of unique product identifiers. We recommend that you periodically evaluate the implemented procedural controls for their effectiveness. You should take appropriate corrective action when indicated by the evaluation or when other events warrant.
程序控制的例子可以包括清理房间内以前的产品材料、产品隔离、部件隔离和使用独特的产品标识符的程序。我们建议您定期评估已实施的程序性控制的有效性。当评估结果显示或其他事件需要时,您应采取适当的纠正措施。
B. Biological and Biotechnological Products (生物和生物技术产品)
1. General Considerations (一般考虑因素 )
The manufacturing process is critical to ensure the correct composition, quality, and safety of biological and biotechnology products. For these products, it can be difficult to distinguish changes in quality attributes, or predict the impact of observed changes in quality attributes on safety. This is especially true for phase 1 clinical trials where knowledge and understanding of a phase 1 investigational drug is limited and where comprehensive product characterization is often unavailable, especially for products that are difficult to characterize. Therefore, it is critical to carefully control and record the manufacturing process in conjunction with appropriate testing to reproduce a comparable phase 1 investigational drug as may be necessary. Properly stored retained samples (e.g., API or drug substance, in-process material, phase 1 investigational drug) that can be subsequently analyzed for comparison, can provide important links in reproducing comparable biological and biotechnological products.
制造过程对于确保生物和生物技术产品的正确成分、质量和安全至关重要。对于这些产品,可能很难区分质量属性的变化,或预测观察到的质量属性变化对安全性的影响。这对于一期临床试验来说尤其如此,因为对一期研究性药物的知识和理解是有限的,而且往往无法获得全面的产品特征描述,特别是对于那些难以描述的产品。因此,结合适当的测试,仔细控制和记录生产过程,以便在必要时重现可比较的1期研究性药物,这一点至关重要。适当储存的保留样品(如原料药或药物物质、加工中的材料、1期研究性药物),可以随后进行分析比较,可以为复制可比的生物和生物技术产品提供重要环节。
You should have in place appropriate equipment and controls in manufacturing to ensure that unit operations with safety-related functions (e.g., viral clearance, virus/toxin attenuation, pasteurization) perform their function with a high degree of assurance. Specific testing may also serve to complement these functions. In manufacturing, you should use testing for safety-related purposes such as viral loads, bioburden, detoxification of bacterial toxins, virus clearance (i.e., removal or inactivation), and removal of residual substances (e.g., antibiotics, chemicals) as appropriate (see section VI.B.2).
您应该在生产中配备适当的设备和控制措施,以确保具有安全相关功能的单元操作(如病毒清除、病毒/毒素衰减、巴氏杀菌)以高度的保证发挥其功能。特定的测试也可用于补充这些功能。在生产中,您应酌情使用与安全有关的测试,如病毒负荷、生物负荷、细菌毒素的解毒、病毒清除(即去除或灭活)和去除残留物质(如抗生素、化学品)(见第VI.B.2节)。
2. Adventitious Agent Control (外来因子控制)
When evaluating the manufacturing environment for biological and biotechnology phase 1 investigational drugs, it is of particular importance to evaluate for susceptibility to contaminate the environment with biological substances, including microbial adventitious agents (e.g., bacterial, viral, mycoplasm), that may remain from previous research or manufacturing activities.
在评估生物制品1期段研究性药物的生产环境时,特别重要的是要评估对生物物质污染环境的敏感性,包括以前研究或生产活动中可能残留的微生物不定型剂(如细菌、病毒、支原体)。
Some biological and biotechnology phase 1 investigational drugs, including those made from pathogenic microorganisms, spore-forming microorganisms, transgenic animals and plants, live viral vaccines, and gene therapy vectors, warrant additional containment considerations. We encourage you to discuss such containment issues with the applicable Center within FDA (i.e., product and facility group with responsibility for the product) prior to engaging in manufacturing.
一些1期生物制品药物,包括那些由病原体微生物、孢子形成的微生物、转基因动物和植物、活病毒疫苗和基因治疗载体制成的药物,需要额外的遏制考虑。我们鼓励您在从事生产之前,与FDA内适用的中心(即负责该产品的产品和设施组)讨论此类遏制问题。
In addition to the recommendation in section VI.A, multi-product facilities should have in place cleaning and testing procedures that ensure prevention and/or detection of contamination by adventitious agents. To the extent possible, we recommend the use of dedicated equipment and/or disposable parts (e.g., tubing) for this reason. For multi-product areas, you should establish procedures to prevent cross-contamination, and to demonstrate removal of the previously manufactured product from shared equipment and work surfaces, especially if live viral and vector processing occurs in a manufacturing area.
除了第 VI.A 节的建议外,多产品设施应具备清洁和测试程序,以确保预防和/或检测外来物的污染。为此,我们建议尽可能地使用专用设备和/或一次性部件(如管道)。对于多产品区,您应该建立防止交叉污染的程序,并证明从共享的设备和工作表面清除先前生产的产品,特别是如果活体病毒和载体处理发生在生产区。
3. Gene Therapy and Cellular Therapy Products (基因治疗和细胞治疗产品 )
Due to the wide variety and unique manufacturing aspects of investigational gene and cellular therapy products, manufacturers should consider the appropriateness of additional or specialized controls. Although you should manufacture phase 1 investigational cell and gene therapy products following the recommendations in this guidance, we recognize that it may not be possible to follow each recommendation. For example, with some cellular products, it may be impossible to retain samples of the final cellular product due to the limited amounts of material available. Therefore, we recommend that you include your justification for adopting additional controls or alternative approaches to the recommendations in this guidance in the records on the phase 1 investigational drug.
由于研究性基因和细胞治疗产品的种类繁多,制造工艺独特,制造商应考虑额外或专门控制的适当性。尽管您应该按照本指南中的建议生产第1期研究性细胞和基因治疗产品,但我们认识到,可能无法遵循每一项建议。例如,对于某些细胞产品,由于材料的数量有限,可能无法保留最终细胞产品的样本。因此,我们建议您在关于1期研究性药物的记录中包括您对本指南中的建议采取额外控制或替代方法的理由。
In some cases, investigational gene and cellular therapy products may be manufactured as one batch per subject in phase 1 clinical trials (e.g., gene vector modified autologous cell products, autologous cell products). Manufacture of multiple batches will allow manufacturing and testing information to accumulate in an accelerated manner as compared to more conventional products. As manufacturing methods and assays used for testing can be novel for these products, it is important to monitor manufacturing performance to ensure product safety and quality.
在某些情况下,研究性基因和细胞治疗产品可以在1期临床试验中为每个受试者制造一个批次(例如,基因载体修饰的自体细胞产品、自体细胞产品)。与更传统的产品相比,多批次的制造将使制造和测试信息加速积累。由于这些产品的制造方法和用于测试的检测方法可能是新颖的,因此监测制造性能以确保产品安全和质量是很重要的。
When manufacturing multiple batches of the same phase 1 investigational drug, we recommend that manufacturers periodically conduct and document internal performance reviews. We recommend that this review assess whether the manufacturing process is optimal to ensure overall product quality. Based on the review, appropriate modifications and corrective actions can be taken to control procedures and manufacturing operations.
当制造同一阶段研究性药物的多个批次时,我们建议制造商定期进行内部绩效审查并记录。我们建议,这种审查应评估制造过程是否最佳,以确保整体产品质量。在审查的基础上,可以采取适当的修改和纠正措施来控制程序和生产操作。
C. Sterile Products/Aseptically Processed Products (无菌产品/无菌加工产品 )
Because product sterility is a critical element of human subject safety, you should take special precautions for phase 1 investigational drugs that are intended to be sterile. You should give thorough consideration to implementing appropriate controls for aseptic processing to ensure a sterile phase 1 investigational drug. The guidance issued by FDA on aseptic processing is a good reference when using aseptic processing (Ref. 7). Particular manufacturing controls include:
由于产品的无菌性是人类受试者安全的一个关键因素,您应该对打算无菌的1期研究药物采取特别的预防措施。您应该充分考虑对无菌加工实施适当的控制,以确保1期研究性药物的无菌性。在使用无菌加工时,FDA发布的无菌加工指南是一个很好的参考(参考文献7)。特别的生产控制措施包括:
-
Conducting aseptic manipulation in an aseptic workstation (e.g., laminar air flow workbench, biosafety cabinets, or barrier isolator system) under laminar airflow conditions that meet Class A, ISO 5. You should perform all manipulations of sterile products and materials under aseptic conditions.
-
Conducting a process simulation using bacterial growth media to demonstrate that the aseptic processing/controls and production environment are capable of producing a sterile drug
-
Performing environmental monitoring of the aseptic workstation during processing to ensure appropriate microbiological control. Such monitoring may include microbial monitoring by settling plates or by active air monitoring.
-
Disinfecting the entire aseptic workstation as appropriate to the nature of the operations (e.g., before aseptic manipulation, or between different operations during the same day)
-
Ensuring proper workstation installation and placement (e.g., workstations sufficiently separated to allow appropriate airflow) and ensuring that items within a laminar airflow aseptic workstation do not interrupt the unidirectional airflow
-
Disinfecting gloves or changing them frequently when working in the laminar flow hood
-
Disinfecting the surface of nonsterile items (e.g., test tube rack, and the overwrap for sterile syringes and filters) with sterile disinfectant solution before placing them in the laminar flow hood
-
Documenting and following all procedures intended to maintain the sterility of the components, in-process materials, and final phase 1 investigational drug
-
Demonstrating that the test article does not interfere with the sterility tests (e.g., USP <71>)
-
Employing aseptic technique and control of microbiological impurities in components designed to prevent microbial and endotoxin contamination
-
Training personnel in using aseptic techniques
-
Verifying that the equipment is suitable for its intended use, i.e., sterilization (e.g., autoclave, hot air oven); performing appropriate calibration of temperature probes used to monitor the sterilization cycle; using suitable and qualified biological indicators; and retaining maintenance and cycle run log records
-
Demonstrating that the sterilization method for sterile components and disposable equipment (e.g., filters, bags, containers/ stoppers) is suitable and creating documentation that supports the appropriate use and shelf life of sterile components and equipment
-
Ensuring that release of the final phase 1 investigational drug by the QC unit, or designated individual, includes an acceptable review of manufacturing records that demonstrate aseptic procedures and precautions were followed
-
Ensuring that final phase 1 investigational drugs are not released until acceptable results of sterility testing are known. We understand that you may have to release a phase 1 investigational drug with a short shelf-life (e.g., radiopharmaceutical, cellular product) based on results from relevant tests (e.g., assessment of sterile filtration by bubble point filter integrity test, cell product — an in-process test result and a negative gram stain, or other rapid microbial detection test and negative endotoxin test on the final product) while results of the sterility test are pending. When you obtain positive results or other relevant results from sterility testing, we recommend that you perform an investigation to determine the cause of contamination followed by corrective action, if warranted. You should notify the person responsible for the associated clinical trials so appropriate action can be taken.
-
在符合ISO 5级的层压气流条件下,在无菌工作站(如层压气流工作台、生物安全柜或屏障隔离系统)进行无菌操作。应在无菌条件下进行无菌产品和材料的所有操作。
-
使用细菌生长介质进行工艺模拟,以证明无菌加工/控制和生产环境能够生产无菌药物
-
在加工过程中对无菌工作站进行环境监测,以确保适当的微生物控制。这种监测可包括通过沉淀板或通过主动空气监测进行微生物监测。
-
根据操作的性质对整个无菌工作站进行消毒(例如,在无菌操作前,或在同一天的不同操作之间)。
-
确保工作站的正确安装和摆放(例如,工作站充分分开,以保证适当的气流),并确保层流无菌工作站内的物品不中断单向气流的运行
-
-
在将非无菌物品(如试管架、无菌注射器和过滤器的外包装)放入层流罩之前,用无菌消毒液对其表面进行消毒处理。
-
记录并遵循所有旨在保持部件、过程中材料和最终一期研究性药物无菌的程序
-
证明试验品不会干扰无菌性测试(例如,USP <71>)。
-
采用无菌技术和控制组件中的微生物杂质,旨在防止微生物和内毒素污染
-
-
验证设备是否适合其预期用途,即灭菌(如高压灭菌器、热风炉);对用于监测灭菌周期的温度探头进行适当的校准;使用合适的、合格的生物指标;保留维护和周期运行记录
-
证明无菌部件和一次性设备(如过滤器、袋子、容器/塞子)的灭菌方法是合适的,并建立文件以支持无菌部件和设备的适当使用和保质期
-
确保质量控制单位或指定的个人对最后1期研究用药的发布包括对证明无菌程序和预防措施得到遵守的生产记录进行可接受的审查。
-
确保在得知可接受的无菌测试结果之前,不释放最终的1期段研究性药物。我们理解,在无菌性试验结果尚未出来之前,贵方可能不得不根据相关试验的结果(例如,通过泡点过滤器完整性试验评估无菌过滤,细胞产品--过程中试验结果和革兰氏染色阴性,或其他快速微生物检测试验和最终产品的内毒素试验阴性)释放保质期较短的1期段研究性药物(例如,放射性药物、细胞产品)。当您从无菌检测中获得阳性结果或其他相关结果时,我们建议您进行调查,以确定污染的原因,然后采取纠正措施(如有必要)。您应通知负责相关临床试验的人员,以便采取适当的行动。
-
FDA guidance on the “Preparation of Investigational New Drug Products (Human and Animal)” 1991 (reprinted November 1992).
-
FDA “Guidance for Industry, Investigators, and Reviewers: Exploratory IND Studies.”
-
FDA “Guidance for Industry: Q7A Good Manufacturing Practice Guidance for Active Pharmaceutical Ingredients,” Section 19.
-
FDA “Guidance for Industry: Content and Format of Investigational New Drug Applications (INDs) for Phase 1 Studies of Drugs, Including Well-Characterized, Therapeutic, Biotechnology-derived Products.”
-
FDA “Draft Guidance for Industry: Instructions and Template for Chemistry, Manufacturing, and Control (CMC) Reviewers of Human Somatic Cell Therapy Investigational New Drug Applications (INDs),” August 2003.
-
FDA “Draft Guidance for FDA Review Staff and Sponsors: Content and Review of Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs),” November 2004.
-
FDA “Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practices.”
 本次直播免费参加,点击上方图片即可快速报名,并预约直播。
本次直播免费参加,点击上方图片即可快速报名,并预约直播。




 个人中心
个人中心
 我是园区
我是园区